Researchers say health officials must be careful about where vaccine is used
By Stephanie Desmon
(Editor’s Note: The dengue virus is carried by the Aedes aegypti mosquito)
The only approved vaccine for dengue may actually increase the incidence of dengue infections requiring hospitalization rather than preventing the disease if health officials aren’t careful about where they vaccinate, new public health research published September 2 in Science suggests.
Dengue typically causes a mild first infection but a far worse one if someone is infected with the virus a second time. There are four types of dengue virus, and it is thought that the body’s response to the first infection leads to more severe disease upon a second infection. This has long posed challenges to scientists developing a vaccine, who worried that any candidate that failed to protect fully could raise the risk of making people sick rather than keeping them well.
In their new study, researchers from the Johns Hopkins Bloomberg School of Public Health, Imperial College London and the University of Florida re-analyzed data from vaccine trials conducted in 10 countries with more than 30,000 participants as well as recently published data on a long-term follow-up with these participants.
Using that data, they developed mathematical models to understand how a vaccine rollout would affect people in countries where transmission of the disease is high, moderate or low. They found that while the vaccine can reduce illness and hospitalization by 20 to 30 percent in places where there is high transmission of dengue, it may actually significantly increase illness and hospitalization if used in locations where there is lower transmission of the virus.
The vaccine, manufactured by Sanofi-Pasteur, has been licensed in six countries so far, and multiple countries are currently considering how to use this vaccine.
“In vaccines, you hope for more than 30 percent success, but it’s the only vaccine available right now to slow dengue,” says Isabel Rodriguez-Barraquer, MD, PhD, MHS, a research associate at the Bloomberg School and one of the study’s lead authors. “If this vaccine is used correctly, many people could be spared illness and hospitalization from dengue. But we should make sure we only use it in places where our data suggest it will do more good than harm.”
The new research suggests that the vaccine acts very much like a natural infection but without making recipients sick. In those who have previously been infected with dengue, the vaccine acts like a silent second infection, stimulating the immune system without the more severe symptoms that may accompany a natural second infection.
In those who have not yet been infected with dengue, the vaccine causes the immune system to recognize that a first dengue infection has occurred and then when exposed to dengue in a natural setting, the body reacts as if it is getting a second infection that may be more severe.
The manufacturers of the three-dose vaccine have acknowledged their vaccine does not work well in people who haven’t previously had a naturally occurring dengue infection before vaccination, the researchers say. The vaccine is not indicated for use in children under age 9 because they are least likely to have been exposed to dengue.
Partly based on these findings, the World Health Organization is recommending that this vaccine be used only in areas where there is a known high burden of disease.
“We should be careful in considering where and how to use this vaccine as there is still uncertainty about its impact,” says Derek A.T. Cummings, PhD, a professor of biology at the University of Florida, an adjunct professor at the Bloomberg School and another of the study’s authors.
The authors hope that their analysis can help inform policymakers in evaluating this and other candidate dengue vaccines.
“Having a vaccine is a significant step forward for dengue control,” Rodríguez-Barraquer says. “However, this vaccine is a prime example of having to seriously weigh the risks and benefits.”
Dengue infects nearly 400 million people across more than 120 countries each year. Most survive with few or no symptoms, but more than 2 million annually develop what can be a dangerous dengue hemorrhagic fever, which kills more than 25,000 people each year.
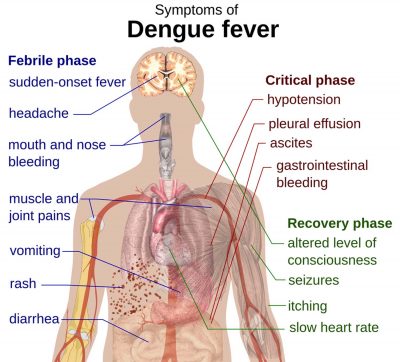
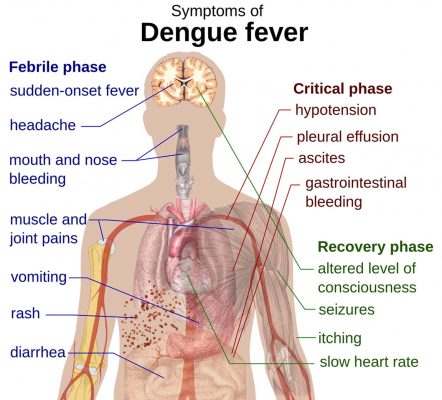
Dengue can cause a high fever, severe headaches, severe pain behind the eyes, rash and joint, muscle or bone pain. Dengue hemorrhagic fever occurs when blood leaks from blood vessels into other parts of the body, which can lead to failure of the circulatory system, shock and possibly death, without prompt treatment.
One thing that could help make decisions easier, the researchers say, would be a blood test that could identify those that have been infected in the past. Those who had been would get the vaccine; those who had not been would not be vaccinated.
The study, Benefits and risks of the Sanofi-Pasteur dengue vaccine: Modeling optimal deployment, was written by Neil M. Ferguson, Isabel Rodriguez-Barraquer, Ilaria Dorigatti, Luis Mier-y-Teran-Romero, Daniel J. Laydon and Derek A.T. Cummings.
The work was funded by the UK Medical Research Council, the UK National Institute of Health Research under the Health Protection Research Unit initiative, the National Institute of Allergy and Infectious Diseases and National Institute of General Medical Sciences under the MIDAS initiative, and the Bill and Melinda Gates Foundation.